Sleep apnea and insomnia are the two most commonly diagnosed sleep disorders. When they occur together in the same person, it’s a special kind of torment called COMISA (Comorbid Insomnia and Sleep Apnea). Fortunately, treatment for sleep apnea and insomnia can be successful when proven therapeutic steps are followed.

COMISA impacts at least a third of people with insomnia or sleep apnea. Acknowledging and naming this condition is an important step in validating a patient’s experience and recognizing the toll it takes, physically, mentally, and emotionally. Successful treatment for sleep apnea and insomnia requires this acknowledgement as the starting point.
Left untreated, the effects of COMISA can be debilitating and additive, with multiple symptoms of poor-quality sleep and impaired daytime functioning. Daytime fatigue is a common symptom, which manifests as reduced productivity, low endurance for daily activities, and mood swings or irritability. Relationships may become strained under the weight of sleep deprivation. Personal well-being falters. Those affected can feel like they never really sleep well – and are never fully awake, either.
As a sleep medicine physician and professional sleep coach, it is my responsibility to help people:
- get healthy and restorative sleep night after night
- reliably experience alertness and vitality in the waking hours
- regain trust in their ability to sleep and feel awake
- get high-touch support for the treatment of sleep disorders
- be prepared with tools and support when sleep challenges come up
Throughout my years of practice in treatment for sleep apnea and insomnia, patients grappling with COMISA have presented a unique challenge. Untangling the sources of sleep disruption and implementing treatments is a tricky endeavor that usually takes more expertise, more diligence, and more time to resolve. For those reading, I hope that this information will help you to advocate for yourself as you partner with a physician or coach to finally get the deep sleep you deserve.
Table of Contents
Diagnosis of Sleep Apnea and Comorbid Insomnia (COMISA)

The coexistence of sleep apnea and insomnia makes diagnosing and measuring the severity of either condition more complex. Insomnia and obstructive sleep apnea share risk factors (primarily obesity and age) and multiple overlapping day/night symptoms, so the possibility that both conditions are operating within the same person is worth considering.
On a backdrop of stress, irregular sleep schedules, excessive caffeine intake, environmental sleep challenges, and underlying health conditions (including depression and anxiety), there is a lot to unpack. Patients with COMISA often present with prominent symptoms of sleep disruption, daytime dysfunction, and a generalized complaint of “I don’t sleep well,” effectively lumping all effects of their sleep disorder together.

Insomnia is an example of how the mind-body connection can go awry, and there are layers of precipitating and perpetuating factors that result in a range of unwanted effects. Approximately 6-10% of the general population suffers from chronic insomnia. This condition is characterized by a state of hyperarousal causing problems getting to sleep and staying asleep.
Hyperarousal can manifest as thinking ruminations, anxiety, increased heart rate, and shallow breathing. A low threshold for arousal can cause a person to spend more time in transitional (light) sleep, and this commonly results in the perception that there has been no sleep at all.
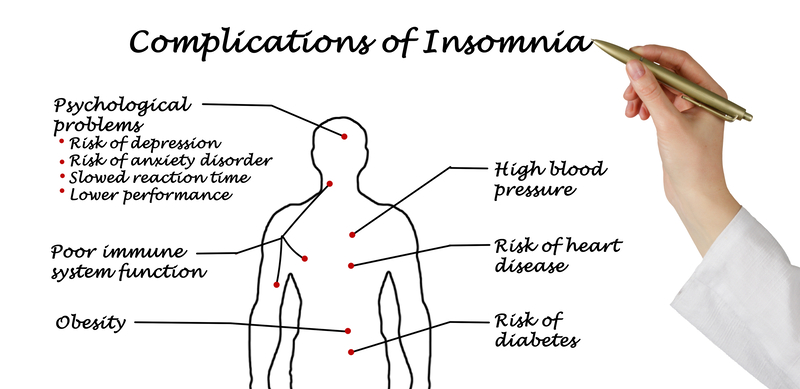
Insomnia is a clinical diagnosis and severity is measured with the Insomnia Severity Index (ISI) questionnaire, which surveys both nighttime and daytime symptoms and yields a number score meant to capture severity. For example, a score equal to or above 15 indicates clinically significant insomnia. Consequences of untreated insomnia include reduced quality of life and long-term health risks related to sleep deprivation.
Sleep apnea, specifically obstructive sleep apnea (OSA), is best characterized as a breathing problem where repeated airway obstructions (due to collapse of the upper airway during sleep) cause drops in blood oxygen levels and sleep disruption. It’s estimated that 80% of people with OSA have not yet been diagnosed. Risk factors include obesity, age, airway and facial anatomy, and some medical conditions.
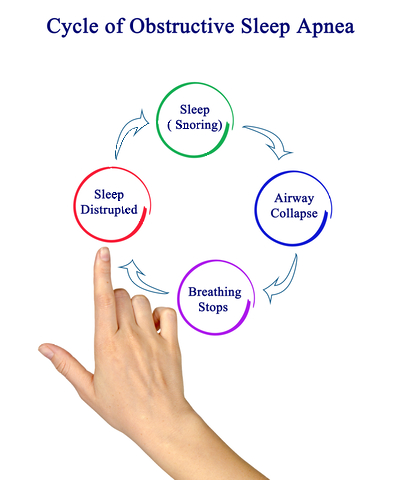
Airway obstructions can occur hundreds of times at night for those with moderate or severe obstructive sleep apnea but may not be perceived by the one with the condition. OSA is associated with increased inflammation, surges in the sympathetic (fight or flight) nervous system, hormonal dysregulation, and metabolic dysfunction. Without treatment for sleep apnea, patients can experience reduced life quality and long-term effects including cardiovascular, metabolic, and neurologic disease.
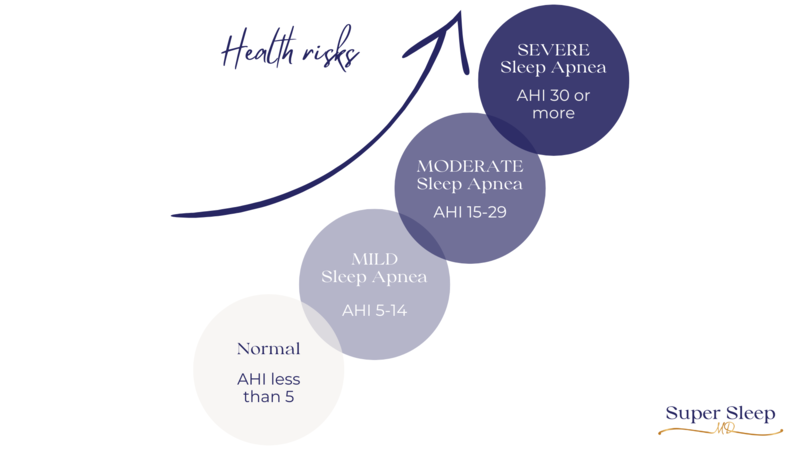
Obstructive sleep apnea severity is measured with the apnea-hypopnea index (AHI), with increasing AHI numbers corresponding to severity. The presence of untreated obstructive sleep apnea and its associated symptoms typically elevates the ISI score because a person with OSA can experience similar daytime symptoms as a person with insomnia.
Conversely, the presence of untreated insomnia can affect the AHI measurement (especially if home sleep apnea testing is used), and both insomnia and OSA are associated with sleep disruption. There is some evidence that partial sleep deprivation can exacerbate OSA. This could suggest an underlying mechanism by which symptoms of each disorder predispose patients to the other.
OSA may contribute to the development or worsening of insomnia. OSA is associated with brief awakenings and surges in heart rate after airway obstruction. This makes sense, because if a person awakens fully, it is often difficult to return to sleep and the perception may be that of insomnia. I frequently point out that untreated OSA is a threat to breathing, sleep, and oxygenation, so it naturally increases hypervigilance. Repeated instances of sleep interruption can quickly turn into frustration which only serves to perpetuate poor sleep and the experience of insomnia.

And then there is Upper Airway Resistance syndrome (UARS). This is a condition in between benign snoring and the lower limit of OSA, and it is not yet fully understood. With UARS, increased resistance of the upper airway (or flow limitation) is present and demonstrated with an in-lab sleep study to cause sleep disruption. A significant number of people with UARS report a lower quality of life despite not having a sleep-related breathing disorder recognized by insurance criteria.
In cases of UARS, the co-existence of insomnia may be associated with a reduced respiratory arousal threshold, which may predispose patients to awaken with smaller degrees of airway narrowing. I have had success in my practice in treating UARS patients with CBT-I (Cognitive Behavioral Therapy for Insomnia) and (self-paid) modes of OSA treatment, including PAP and oral appliance therapy.
Insomnia may exacerbate the severity of sleep sleep-disordered breathing. Conversely, the presence of sleep apnea can contribute to the development and worsening of insomnia. COMISA affects the diagnosis and determination of severity for both conditions. More importantly, the intricate dance between insomnia and sleep apnea necessitates a personalized, holistic, and responsive approach to treatment.
Treatment for Sleep Apnea and Comorbid Insomnia (COMISA)
Many sleep medicine specialists elect to start with treatment for sleep apnea first and then determine if insomnia symptoms are left over. In my experience, this can result in a dramatic worsening of the patient’s condition. People with COMISA rightly perceive that their sleep is fragile and adding OSA therapy to untreated insomnia results in further decline of sleep quality and significantly greater impairment of daytime functioning. This typically leaves a person feeling incredibly discouraged about their ability to have healthy sleep. So discouraged, in fact, that they may abandon care altogether.
In the course of a sleep apnea evaluation, there is an opportunity to address insomnia first. Insomnia treatment can start while a patient is waiting for their sleep test or waiting for their OSA treatment. The first-line treatment for insomnia is CBT-I (Cognitive Behavioral Therapy for Insomnia). This may be delivered by appropriately trained clinicians or sleep coaches. Regular interactions in as little as 4-6 weeks can be incredibly effective.
First-line treatment for sleep apnea (moderate to severe) is with Positive Airway Pressure (PAP, such as CPAP, AutoPAP, and other PAP modalities), which requires acclimation to the mask and pressure with nightly use for resolution of OSA. It is important to note that initial CPAP acceptance and use predicts future CPAP use, especially within the first month of CPAP.

In other words, a positive initial experience with CPAP therapy encourages and maintains greater long-term adherence. However, for people who didn’t have a good experience with CPAP but are still motivated to treat their sleep apnea, I’ve found that effective use of CPAP can absolutely be achieved in the treatment for sleep apnea through coaching, support, and education.
Those with COMISA are often less accepting of PAP therapy (even compared to people with OSA alone), which can understandably trigger hypervigilance — a barrier to acclimation to the mask and air pressure. Short-term use of prescription sleep aids, lifestyle modifications (including active stress reduction), and behaviors to engage the parasympathetic (rest and digest) nervous system can be personalized to promote acclimation to CPAP while still supporting sleep quality and quantity.

This requires trust, good communication, and frequent follow-up between the person with COMISA and their clinician or coach. Given the lack of access to sleep medicine providers, this work may fall to a sleep coach for a high-touch and personalized plan.
Non-CPAP therapies can and should be considered in the COMISA population. Non-surgical treatments (especially oral appliance therapy, or OAT) and surgical procedures for OSA are options. Selection of a CPAP treatment alternative is dependent on patient preference, the severity of OSA, co-existing medical conditions, and cost or insurance coverage. It is my practice to caution COMISA patients about hypoglossal nerve stimulation surgery because the implant for OSA can exacerbate insomnia.
For more guidance, watch my video interview about sleep apnea treatment alternatives without CPAP:
There is precedent for hope in the treatment for sleep apnea and insomnia. Research shows that those receiving both effective CBT-I and CPAP therapy report significantly greater improvement of global insomnia symptoms and meaningful sleep apnea treatment by 6 months follow-up.
In summary, people with COMISA require a higher level of expertise, more frequent care, and targeted diagnostic and therapy considerations. Insomnia therapy should occur at least simultaneously (or preferably before!) a sleep apnea evaluation. Insomnia should not be assumed to be a ‘secondary’ manifestation of OSA.
Left unaddressed, underlying insomnia can significantly impair a person’s ability to function as they begin treatment for sleep apnea, and a savvy clinician will pivot accordingly. Flexibility in choices for OSA therapy should be the norm, and frequent and personalized follow-up visits would be ideal for support and troubleshooting.
Frequently Asked Questions
How can I acclimate more quickly to CPAP?
Consistency is key when you are getting into the habit of using CPAP therapy! The goal is to wear your CPAP throughout the night so you can have normal breathing during sleep. But few people can achieve this from the very first night!
If you are new to CPAP or coming back to it after a break, plan to use the treatment nightly for best results. Use CPAP for as long as you can each night, but don’t get discouraged if you can’t make it through the whole night at first. You can work up to it over time. Set your mask on top of your pillow so you see it every night. Clean the mask in the morning and get your equipment ready for the next use.
If you experience anxiety or agitation with CPAP at night, then practice using your mask during the day when there is no pressure to sleep. Put on your mask and wear it for at least 15 minutes while reading, looking at your phone, or watching TV. This helps to teach your brain that the mask is safe and familiar. Add the tubing and air pressure and increase the time until you feel neutral about the experience.
What is combination therapy?
Combination therapy describes using multiple treatments for sleep apnea and other sleep problems. There are many tools for treating all combinations and contributors to sleep diagnoses, so let’s get creative in using them! Here are some examples:
• Use CPAP while embarking on a weight loss journey
• Use CPAP with a prescription sleep aid during the acclimation phase (30-60 days)
• Use CPAP with an oral appliance to reduce the air pressure needed to treat sleep apnea
• Use CPAP and position therapy to reduce the air pressure needed to treat sleep apnea
• Use CPAP routinely at home and oral appliance therapy when traveling
• Use an oral appliance for sleep apnea in combination with sleep position therapy
• Layered surgical treatments to open up the nose and/or throat
What other treatment options are there for Obstructive Sleep Apnea (besides CPAP)?
CPAP is the gold standard for the treatment of OSA because it is effective more than 95% of the time. However, one must be using the treatment for it to be effective! For those who are looking for other treatments besides CPAP, I invite you to check out my online course called 21+ CPAP Alternatives. I have divided the material into surgical and non-surgical options, and have included information about patient eligibility, success rates, cost, and side effects. Know your options so you can decide what will work for you!
Is sleep coaching covered by insurance?
At this time sleep coaching is not covered by insurance, although using HSA or FSA funds may be an option. Every insurance plan is different; check your own policy to determine what you are eligible for.
Is it okay to take a sleeping pill with CPAP?
A diagnosis of insomnia with sleep apnea (COMISA) is a situation that may warrant the use of a prescription sleep aid. In general, sleeping pills should be considered temporary but can be helpful during the acclimation phase of CPAP. If you have untreated obstructive sleep apnea and you take a sleeping pill, your arousal to breathe may be more difficult. Consequently, you may stop breathing for longer periods and have bigger drops in your blood oxygen levels. The decision to take a sleeping pill is best made in collaboration with your prescribing physician.
Dr. Audrey Wells, Super Sleep MD
I'm Dr. Wells, a sleep medicine physician. I can show you how to get comfortable with CPAP or move on to a different treatment.
More: https://sleepcoaching.com/super-sleep-md-audrey-wells/


Thank you for this informative article on treating sleep apnea and insomnia. It’s encouraging to see such comprehensive coverage of both conditions, particularly the emphasis on holistic approaches alongside traditional treatments.
I found the section on lifestyle changes particularly enlightening. It’s often easy to overlook the impact of daily habits on sleep quality.
However, I was hoping to see more on the role of technology in monitoring and improving sleep, like smart wearables and sleep tracking apps. In my experience, they can be quite helpful in understanding sleep patterns.
Also, I think adding some user experiences or case studies could make the information more relatable. Overall, a great read that offers valuable insights for anyone struggling with these sleep issues.
Dr. Wells, your insightful article on “Effective Treatment for Sleep Apnea and Comorbid Insomnia (COMISA)” serves as an essential guide for those grappling with these challenging conditions.
Your deep dive into the complexities of diagnosing and treating COMISA is impressive. The emphasis on the need for personalized and holistic sleep solutions resonates strongly with anyone who has faced the double challenge of sleep apnea and insomnia. The detailed explanation of the symptoms and risks associated with these conditions, and your expert insights into the latest sleep medicine approaches, make this article a valuable resource for both patients and practitioners.
Moreover, the focus on “sleep apnea treatment” and “insomnia therapy” as integral parts of managing COMISA is particularly enlightening. The inclusion of practical advice and therapeutic options offers hope and guidance to those seeking relief. Your article not only educates but also empowers readers to seek effective treatment, and it stands out as a testament to the advancements in sleep medicine and COMISA management.
Hi there. I used to be a sufferer of insomnia. That was before I found cannabis. Fortunately I have not suffered from sleep apnea but people in my family do. So, it could be something I develop as I grow older.
I think this article will help many people, and possibly even me one day. I definitely look forward to reading more of your content! Thanks!
Dr. Audrey Wells’ article on COMISA effectively highlights the challenges of dealing with both sleep apnea and insomnia. The piece emphasizes the need for personalized treatment, suggesting that addressing insomnia alongside or before sleep apnea evaluation is crucial. Dr. Wells provides practical insights into potential challenges and solutions for COMISA patients, making the article a valuable resource for individuals and healthcare professionals dealing with these coexisting sleep disorders.
Thanks for sharing this. Many conditions people suffer from seem like a cruel trick by nature, and this has got to be up the list. Insomnia is no joke as it is, but when patients with COMISA finally do fall asleep, they suffer from sleep apnea as well. Glad there are professionals like yourself to help diagnose and treat these people!
Hi Dr. Audrey Wells,
I just finished reading your article on the treatment for sleep apnea and comorbid insomnia (COMISA). It’s impressive how you dissect the complexities of these conditions, especially the interplay between them. Your emphasis on the need for a personalized approach to treating COMISA is enlightening and feels like a breath of fresh air in medical treatment discussions.
What I’m thinking about is the role of lifestyle changes in managing COMISA. You mentioned CBT-I and CPAP therapy, but how significant are diet, exercise, and stress management in this context? Could these be as pivotal as the treatments you’ve mentioned?
Thank you for your work and sharing.
Best regards,
Makhsud
Hi, Dr. Wells. Thank you very much for this comprehensive post about sleep apnea and insomnia. I suspect that I have sleep apnea because my wife says that I am snoring and my breath halts for a while during sleeping. I have high blood pressure. Could the apnea cause it?
Alternative treatments to CPAP for sleep apnea is interesting. It’s good to know that there are options available, I think I would struggle to use this machine.
Dove into this piece on treating sleep apnea and comorbid insomnia, and it hits close to home. The struggle with these two sleep disorders can be exhausting, and the article’s approach to addressing them together is like a lightbulb moment.
Personally, I’ve grappled with sleep issues, and the idea of a more integrated treatment plan seems like a game-changer. It’s refreshing to see a focus on comprehensive solutions that consider the interconnected nature of these sleep challenges.
Wow, I had no idea that it was even possible for one to suffer from Sleep Apnea AND Insomnia simultaneously. As of late, sleep and I have had a headbutting relationship to say the least, and this has certainly given me a lot to think about. Thank you for touching on the many proper treatment methods for these conditions Dr. Wells!
This is a very helpful and insightful explanation of sleep apnea and chronic insomnia. It is interesting to see that you say that the two conditions should be treated simultaneously, and ideally treatment for insomnia should be started first.
My sister used to be obese and was suffering from sleep apnea and used to sleep with what she called “the contraption” on her head every night. After losing more than 60% of her weight, she is no longer diabetic, or suffering from sleep apnea. I will share this post with her and the insomniacs that I know.
This is a serious topic and one close to me. It is incredibly hard seeing someone go through these things and it does take a massive toll on them and those around them. That’s why I think this post is such a good one, outlining the diagnosis and complications and showing a way forward for those struggling. A great post about a very serious issue a lot of people and their families are facing!
Having both sleep apnea and insomnia, known as COMISA, is a tough experience – I have not experienced sleep apnea, but I do suffer from insomnia, so the sentiment is there.
I learned that acknowledging and treating these conditions simultaneously is crucial for better outcomes. Untangling the complexities of COMISA requires a personalized approach, focusing on insomnia first before addressing sleep apnea.
It’s understandable that successful treatment involves trust, good communication, and frequent follow-up between the individual and their clinician or coach. This is a journey that demands expertise, diligence, and a commitment to improving both sleep quality and overall well-being. It may not be something that everyone can achieve, but one must certainly try considering the seriousness of this condition.
Thank you for breaking down this important topic!